Upcoding and unbundling are two of the most common and costly forms of healthcare fraud in the United States. These deceptive billing practices involve manipulating the codes submitted to Medicare, Medicaid, or private insurers to inflate reimbursement. While the schemes may appear subtle on paper, their consequences are far-reaching: billions of dollars lost each year, erosion of trust in the healthcare system, and misallocated resources that could otherwise support legitimate patient care.
For healthcare professionals – especially those involved in coding, billing, or direct patient care – understanding what these terms mean is more than just a compliance requirement. It’s a critical step toward protecting the integrity of the healthcare system and ensuring patients receive appropriate and honest treatment.
This article is designed for healthcare providers, billing professionals, administrators, and others working in the healthcare sector who may encounter fraud firsthand. If you suspect unethical billing practices in your organization, this guide can help you identify red flags, understand your rights under the law, and take steps to report misconduct safely and effectively.
What is Upcoding?
Upcoding occurs when a healthcare provider submits billing codes for diagnoses, procedures, or services that are more serious, complex, or time-consuming than what was actually provided. These inflated codes result in higher reimbursement from Medicare, Medicaid, or private insurance – essentially charging more for care that wasn’t delivered at that level.
Billing codes are the backbone of the healthcare reimbursement system. Each service or procedure is assigned a specific Current Procedural Terminology (CPT) or diagnosis (ICD) code. These codes are used to determine how much a provider is paid. With thousands of codes in the system and frequent updates, there’s ample opportunity for misuse – whether intentional or not.
Common Examples of Upcoding:
- Overstating visit complexity: Using a code that indicates a comprehensive evaluation when the visit was brief or routine.
- Misrepresenting procedures: Billing for a complex surgery when only a minor outpatient procedure was performed.
- Inflating time spent: Using Evaluation & Management (E/M) codes that reflect longer or more involved patient visits than actually occurred.
- Improper use of modifiers: Adding codes that suggest additional, distinct procedures were done, when they were actually included in the base service.
Even small discrepancies in coding can add up to significant overpayments especially in high-volume practices, hospitals, or systems that rely heavily on automated billing workflows.
In the context of Medicare and Medicaid, upcoding is considered fraud. It diverts taxpayer-funded resources away from genuine care and undermines the integrity of public health programs.
What is Unbundling?
Unbundling, sometimes called fragmentation, is another common form of healthcare billing fraud. It involves billing separately for services that are normally grouped together under a single code – a practice that artificially inflates the total reimbursement a provider receives.
Medicare, Medicaid, and many private insurers use bundled payment models to reimburse for certain procedures or services that are typically performed together. These bundles are designed to encourage efficiency, reduce redundancy, and limit excessive billing. When a provider breaks apart these bundled services and bills each component individually, they may receive more money than they are entitled to – even though no extra work was done.
Examples of Unbundling:
- Billing separately for a surgical incision and closure that are normally included in the standard code for the procedure.
- Submitting individual codes for a panel of lab tests that are usually reimbursed as a group.
- Charging for post-operative visits that are already covered under a global surgical package.
This type of billing manipulation can significantly inflate costs without improving patient outcomes – and in some cases, without the patient even realizing anything was out of the ordinary.
Unbundling is often difficult to detect from the outside. It frequently requires insider knowledge – someone who understands what should have been billed and noticed when something doesn’t add up.
How Electronic Health Records (EHRs) Can Enable Upcoding and Unbundling
While Electronic Health Record (EHR) systems have improved the accuracy and efficiency of medical documentation, they can also be misused to facilitate fraudulent billing – often without drawing much attention. When combined with bad intent or poor oversight, these tools can make it easier to commit upcoding, unbundling, and other types of healthcare fraud.
Here are some common EHR-Related Practices That Enable Fraud:
Copy-Paste Documentation – Providers may copy notes from a previous visit and paste them into the current visit’s record, making it appear as though more diagnoses were addressed or services were provided than actually occurred.
Limited Code Menus – Some EHR systems may be set up – either by default or by design – to only display procedure or diagnosis codes with the highest reimbursement rates. This can lead to inappropriate code selection or limit staff visibility into correct billing options.
Auto-Populating Notes – Templates that auto-fill sections of a patient’s chart may inadvertently (or intentionally) document services that weren’t actually performed, supporting a falsely inflated claim.
Insufficient Audit Trails – Some systems don’t clearly track who made changes to records or when, making it harder to detect fraudulent edits or retroactive justifications for billing decisions.
While EHRs are meant to streamline care and improve accuracy, they can also create a convenient cover for inflated billing – especially in high-volume practices where oversight is limited. Identifying these patterns often requires someone inside the system to raise concerns.
Who Commits Upcoding?
Upcoding and unbundling can occur across nearly every corner of the healthcare system from individual physicians to large hospitals, urgent care clinics, and even suppliers of medical equipment. These fraudulent billing practices aren’t tied to one specialty or setting; instead, they reflect a broader pattern of manipulating medical coding for financial gain.
Physicians and Medical Specialists
Doctors – including general practitioners and specialists like dermatologists, psychiatrists, orthopedists, and pain management providers – are frequently involved in upcoding. Common examples include billing for more complex patient visits than actually occurred, exaggerating the level of procedures performed, or using modifier codes to falsely suggest distinct services were provided during the same visit. Even small discrepancies in Evaluation and Management (E/M) codes can lead to substantial overpayments when repeated across many patients.
Hospitals and Inpatient Facilities
Hospitals may engage in upcoding by inflating the severity of a patient’s condition in order to receive higher reimbursement through Medicare’s Diagnosis-Related Group (DRG) system. For example, billing for conditions like sepsis or acute respiratory failure – even when not fully supported by clinical evidence – can drastically increase payments. Hospitals have also been found to bill as though care was provided by a physician when it was actually delivered by a nurse practitioner or physician assistant, which is reimbursed at a lower rate.
The Office of Inspector General (OIG) has raised concerns about short inpatient stays that were nonetheless billed at the highest severity level. In 2019, hospitals billed Medicare at the highest severity level for 40% of all 8.7 million inpatient cases – costing over $54 billion. In many cases, the patients’ relatively short stays suggested they were not as sick as claimed.
Other Providers and Suppliers
Fraud isn’t limited to doctors and hospitals. Home health agencies may overstate the time or complexity of in-home visits. Urgent care centers might bill for extensive evaluations or tests that weren’t medically necessary. Durable medical equipment (DME) suppliers have been caught billing for high-cost items never delivered, or for equipment more expensive than what was actually provided.
Real-World Examples of Upcoding Cases
Uncovering upcoding and unbundling schemes often requires the courage and insight of insiders – employees, billing staff, or clinicians – who recognize fraudulent practices and choose to speak up. Thanks to whistleblowers and the protections of the False Claims Act, several major healthcare providers and companies have been held accountable in recent years. Here are a few noteworthy examples:
List a few settlements and cases:
CareAll Management LLC – $25 Million Settlement
A Tennessee-based home health provider, CareAll paid $25 million to settle allegations that it submitted false claims to Medicare and Medicaid. According to the complaint, the company exaggerated the severity of its patients’ conditions and billed for medically unnecessary services to increase reimbursement. The whistleblower in this case, a former employee, filed a qui tam lawsuit that led to the federal investigation and recovery.
EndoGastric Solutions – $5.25 Million Settlement
EndoGastric Solutions, a medical device manufacturer, agreed to pay $5.25 million to resolve allegations that it encouraged healthcare providers to submit inflated claims for procedures involving its surgical device. Although the device could be implanted using a less invasive, lower-cost method, EndoGastric allegedly promoted the use of billing codes for more invasive (and better-reimbursed) procedures. The fraudulent billing guidance came to light through a whistleblower who filed under the False Claims Act.
NextCare Inc. – $10 Million Settlement
NextCare, an urgent care provider with locations across multiple states, paid $10 million to settle claims that it overbilled federal and state healthcare programs. Allegations included inflating the complexity of patient visits and performing medically unnecessary services, such as redundant allergy testing. The case was brought forward by former employees who had firsthand knowledge of the company’s billing practices.
These cases demonstrate how critical whistleblowers are in the fight against healthcare fraud. Without insiders stepping forward, many upcoding schemes would remain hidden – continuing to siphon taxpayer dollars and undermine the integrity of the healthcare system.
Reporting Healthcare Fraud Under the False Claims Act
For those working in the healthcare sector, witnessing fraud – like upcoding or unbundling – can place you in a difficult position. Fortunately, the False Claims Act (FCA) provides a legal pathway for individuals to report fraud against the government while protecting themselves from retaliation and even sharing in any financial recovery.
The False Claims Act is the federal government’s most powerful tool for combating fraud in programs like Medicare, Medicaid, and TRICARE. It allows private individuals (often employees or former employees) to file a lawsuit on behalf of the government when they have evidence of fraud. These lawsuits are called qui tam actions.
Once filed, the lawsuit is kept under seal while the U.S. Department of Justice investigates the claims. If the government intervenes and recovers funds – either through a settlement or court ruling – the whistleblower may receive 15% to 30% of the recovered amount as a reward.
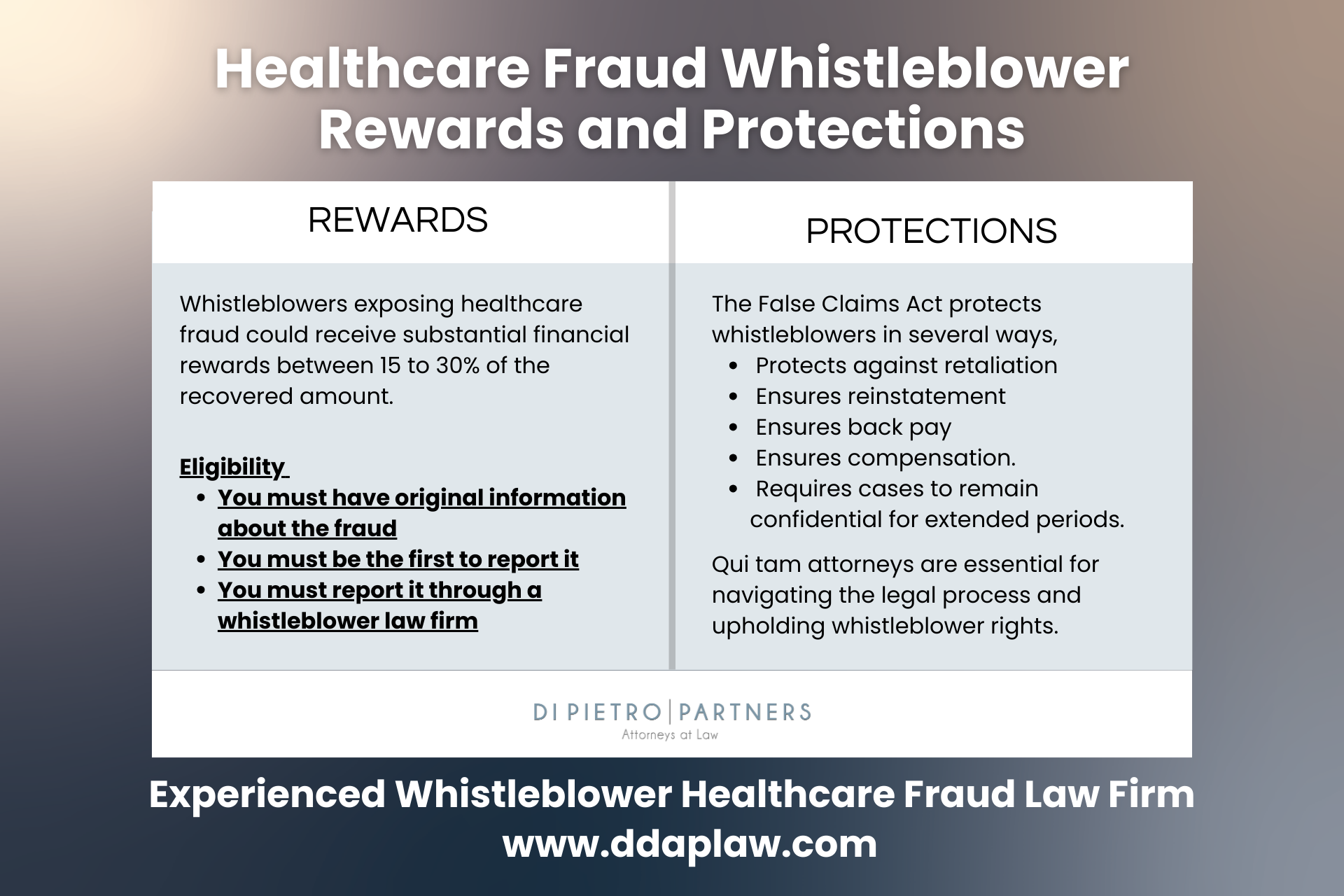
Whistleblower Protections
The FCA also contains strong anti-retaliation provisions. It is illegal for an employer to fire, demote, harass, or otherwise discriminate against an employee for filing a whistleblower claim. If retaliation does occur, the employee may be entitled to compensation, including:
- Reinstatement to their job
- Double back pay
- Compensation for legal fees and emotional distress
Why Legal Guidance Matters
Because filing a qui tam lawsuit is a complex legal process with significant consequences, it’s critical to work with an attorney who specializes in healthcare fraud and whistleblower law. An experienced whistleblower lawyer can help you:
- Document your concerns properly
- File your claim confidentially
- Protect your job and professional reputation
- Maximize your potential reward


