Medicare Integrity Program (MIP) contractors play a pivotal role in safeguarding the integrity of the Medicare program. Their core mission is to prevent, identify, and combat fraud, waste, and abuse within Medicare, ensuring that the program remains sustainable and trustworthy for its beneficiaries. These contractors are tasked with a range of activities including auditing Medicare claims, identifying overpayments, conducting investigations into potentially fraudulent activities, and implementing corrective actions when necessary.
Types of MIP Contractors
Medicare Administrative Contractors (MACs) – These entities process Medicare Part A and Part B medical claims. Their responsibilities include paying claims, collecting Medicare taxes, and providing customer service to beneficiaries. In addition, they perform medical review, which involves ensuring that the claims paid are for services that are covered, correctly coded, and medically necessary.
Zone Program Integrity Contractors (ZPICs) and their successor Unified Program Integrity Contractors (UPICs) – These contractors focus specifically on identifying cases of suspected fraud, waste, and abuse. They conduct in-depth investigations, develop cases for potential prosecution, and take administrative actions when appropriate. UPICs, in particular, integrate the work of ZPICs and the Medicare-Medicaid Data Match Program (Medi-Medi) to provide a more coordinated approach to combating fraud, waste, and abuse across Medicare and Medicaid.
Recovery Audit Contractors (RACs) – These contractors are responsible for identifying and correcting improper payments. They review claims on a post-payment basis, identifying overpayments and underpayments, and implementing corrections to recover overpaid amounts or reimburse underpaid amounts.
Supplemental Medical Review Contractor (SMRC) – Tasked with conducting nationwide medical reviews as directed by the Centers for Medicare & Medicaid Services (CMS), the SMRC addresses issues that pose the greatest risk to the Medicare Trust Funds, such as widespread billing errors or unnecessary services.
These contractors use a variety of tools and methods to fulfill their roles, including data analysis, audits, on-site reviews, and beneficiary interviews. By identifying and rectifying improper payments, they help maintain the financial health of the Medicare program. Furthermore, their efforts in combating healthcare fraud contribute to the protection of Medicare beneficiaries from potentially harmful practices and preserve the integrity of the Medicare system.
Medicare Integrity Program History
The Medicaid Integrity Program (MIP) was initiated by the Deficit Reduction Act of 2005 as the first federal effort dedicated to combating fraud, waste, and abuse in the Medicaid program. Before the MIP, such responsibilities were primarily managed by individual state Medicaid agencies with varying degrees of federal involvement.
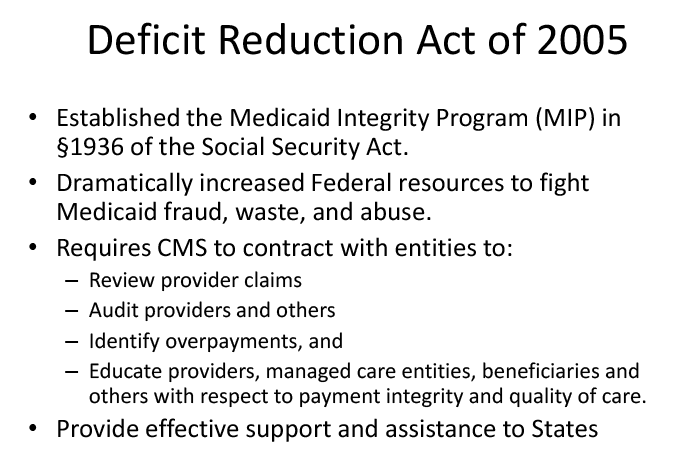
The establishment of the MIP marked a significant step towards a coordinated, nationwide strategy to protect Medicaid’s integrity, introducing federal resources and authority to support, audit, and enforce integrity measures across states.
This approach included hiring contractors to audit Medicaid providers, review Medicaid data for signs of fraud, and educate providers and state officials on best practices for preventing fraud. Over time, the MIP has evolved, incorporating advanced technologies and methodologies to improve its effectiveness in safeguarding Medicaid resources.
